Eczema also known as atopic dermatitis (AD) is a chronic inflammatory disease of the skin. It can cause extreme itching, discomfort and lesions on the skin. Eczema seems to be on the rise, affecting 20% of people worldwide with the majority living in industrialised countries such as Australia and New Zealand. Eczema typically looks like a rough red rash that doesn’t have well defined edges (although there are some types that look a little different). It is characterised by the extreme itching, inflammation and dry skin but can also be blistered, weepy and infected. It typically is on the back of joints, necks, eyelids, palms, fingers, earlobes and scalp (can also affect the face and other areas on some people). Eczema has a huge impact on quality of life for individuals and their families. The itchiness, scaling and lesions of eczema affect sleep quality, create irritation, and can affect self- esteem and self-image. Complications can also arise from this skin condition when the lesions get infected, or further development of allergies such as asthma and hay fever and psychological and behavioural issues.
The pathogenesis of atopic eczema includes a combination of factors which include impaired skin barrier function, IgE-mediated and T-Cell-mediated immune hypersensitivities to food, environment and airborne allergens. Factors involved in the development of IgE mediated allergic disease can be genetic, nutritional, environmental exposures and dysbiotic intestinal microbiota.
Dysregulated immune reactions are a key to start looking at the collection of microbes that live in our gut and intestinal inflammation. We can react because the “good” bugs are out of balance with the “bad” bugs or in the wrong place at the wrong time. What this can cause is inflammation because of the metabolites they produce as they go about their lives or fermenting of foods in different areas of the intestines. Because our immune systems are so closely related to our gastrointestinal systems this can cause upstream effects such as skin issues. This is one of the reasons it is so important to go see a healthcare practitioner who is experienced in these areas. They may recommend further testing to assess gut function and/or food allergens and intolerances that may be creating further inflammation and causing some of these immune responses.
Impaired skin barrier is the other important aspect of managing this condition, the studies show that those who experience eczema often have higher levels of Staphylococcus aureus on their skin than those who do not have eczema. This bacteria colonises the skin and gives off toxins that further impede skin healing and good barrier function. This is an important facet to address when thinking about treatment of eczema and especially with any topical treatments that may be recommended for the condition. Lifestyle: reducing any environmental triggers can be a key part of treatment for this condition. Avoiding topical irritants can include assessing cosmetic, body and cleaning products and avoiding those that have synthetic fragrances, chemicals and essential oils. Cotton sheets and clothes are less irritating than synthetic and wool. Laundry detergent can also be a big trigger so doing an extra rinse during the washing cycle or switching to a more sensitive friendly detergent. Keeping the house as dust free as possible can also reduce exposure to dust mites which can trigger eczema. Some tips that can help are using microfibre cloths to attract more dust, washing sheets regularly and vacuuming to reduce dust mite populations.
Food:
An important part of managing this condition is maximising foods that have a high nutrient intake especially of nutrients that are anti-inflammatory, anti-allergic and wound healing. Food groups that are helpful to include are a rainbow of fruit and vegetables, nuts and seeds, seafood, lean red meat.
Nutrients to include:
• Omega 3 and essential fatty acids – avocado, fish,
• Vitamin A & E – butter, carrots, green leafy vegetables, egg yolk, almonds
• Vitamin C – tomatoes, citrus, kiwi fruit, parsley (best levels are uncooked)
• Vitamin D – safe sunshine exposure, fish liver oils, butter
• Iron – red meat, legumes, nut and seeds, kale, spinach, oats
• Selenium – brazil nuts, oysters, peanuts, onions, alfalfa, wholegrains
• Zinc – beef, capsicum, egg yolk, sunflower & pumpkin seeds, seafood
• Quercetin – apples, broccoli, green tea, buckwheat, garlic, raspberries, red onion
Herbal treatments:
Chamomile extract: Matricaria recutita is an anti-inflammatory, immunostimulant, antibacterial and mild sedative herb. The topical ointment has been found to be more effective than a low dose hydrocortisone cream at relieving the itch and presentation of the lesions. Chamomile can be used as a tea or liquid extract to relieve stress and improve sleep alongside other treatments to improve outcomes.
St John’s Wort extract: Hypericum perforatum has been used as so topical treatment for its activity against Staph. aureus colonisation, used twice daily for 4 weeks it also improved the presentation of eczema lesions. St John’s wort is wound healing, anti-inflammatory and pain relieving as well as antibacterial.
Gotu Kola: Centella asiatica is a lovely wound healing and anti-inflammatory herb that
applied topically can assist with healing and resolution of eczema. Gotu kola can be a really
lovely herbal for the nervous system to reduce stress when taken as a tea or herbal tincture.
Probiotic strains that can be helpful:
Lactobacillus salivarius LS-01 significantly improved eczema scores after 8 weeks of supplementation and was shown to modify the microbiome.
Bifidobacterium breve 16-V has been shown to regulate T-helper cell expression and change the microbiome by maternal supplementation of this probiotic.
There are a range of things to consider when treating this condition including nutritional supplementation and diet, gut microbiome modulation and herbal treatments both topical and internal. Seeing an experienced practitioner who is able to look at the whole picture and formulate a plan including further testing, lifestyle and diet modifications and specific treatments for your individual case is a fantastic way to get on top of this condition and start living your best life.
(References available on request)

Written by Gemma Wells, Naturopath.
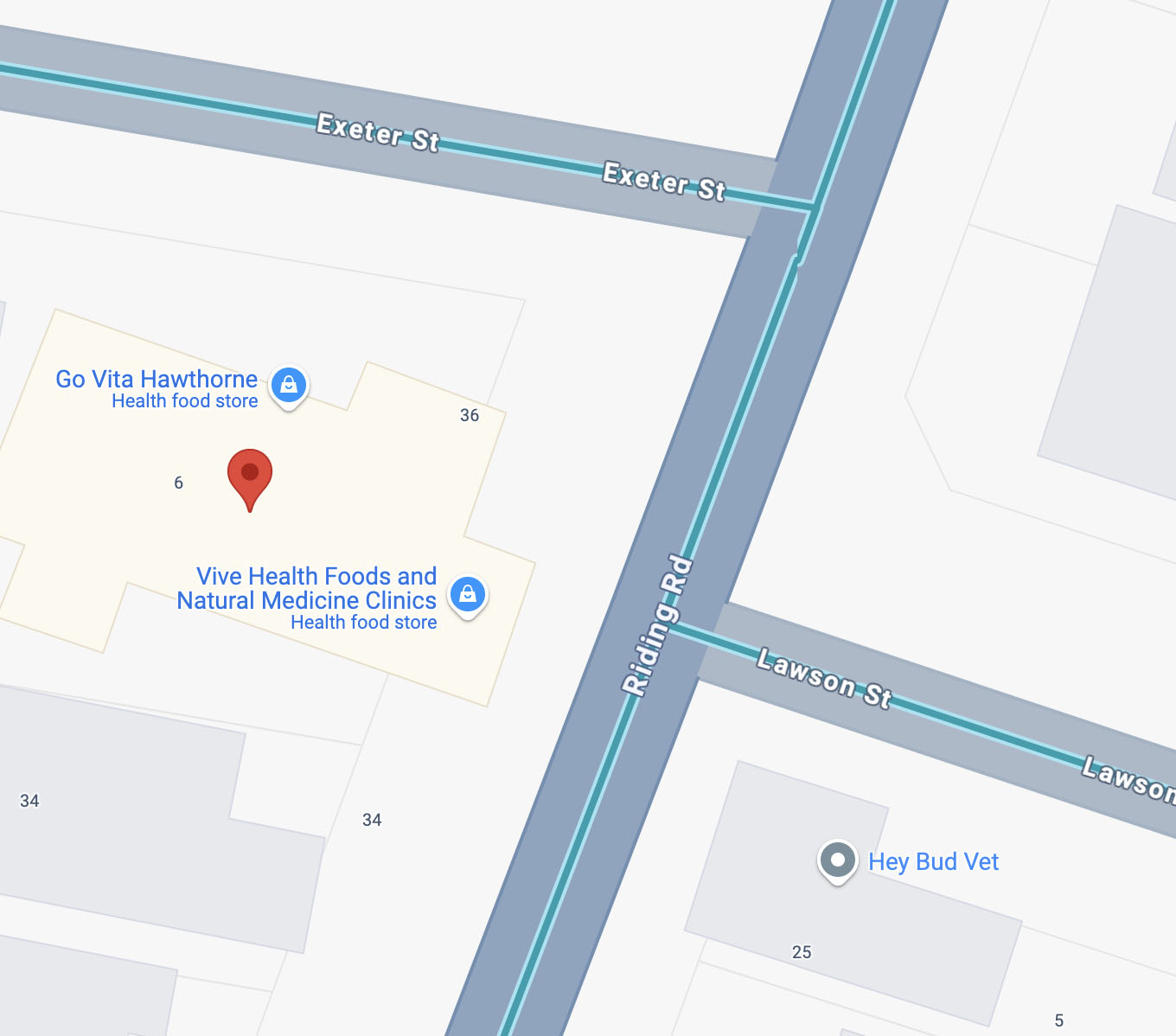
Gemma is available for appointments at the Vive Health Clinic, to book click here.