While the phrase “leaky gut” can mean different things to different people, the underlying concept it refers to—increased intestinal permeability—is well recognised and increasingly studied. The gut lining plays a critical role in how we absorb nutrients, interact with microbes and defend against potential threats—so when this barrier becomes compromised, it can have ripple effects throughout the body.
While the phrase “leaky gut” can mean different things to different people, the underlying concept it refers to—increased intestinal permeability—is well recognised and increasingly studied. The gut lining plays a critical role in how we absorb nutrients, interact with microbes and defend against potential threats—so when this barrier becomes compromised, it can have ripple effects throughout the body.
So, what do we actually know about intestinal permeability? How does it affect our health—and how can we support the gut barrier in meaningful ways?
What is intestinal permeability?
Your gut lining isn’t just a passive tube—it’s a selectively permeable barrier. Its job is to absorb nutrients while keeping toxins, microbes and undigested particles out of the bloodstream.
This selective permeability is tightly regulated under healthy conditions. The barrier itself is a complex, living interface between your body and the outside world—supported by immune defences, microbial allies (microbiome) and protective layers that work together to control what gets through. When functioning well, it allows the selective absorption of beneficial compounds while maintaining a strong defence against potentially harmful substances.
When things go wrong
“Leaky gut” refers to a loss of that selective control. The more accurate term is increased intestinal permeability—when the tight junctions between cells become too loose, allowing unwanted substances to pass into the bloodstream.
This can lead to immune activation, low-grade inflammation and, in some cases, contribute to symptoms such as
- bloating or digestive discomfort
- fatigue or brain fog
- food sensitivities
- skin issues
- systemic inflammation
But increased permeability doesn’t always cause symptoms on its own—it’s often one piece in a broader picture.
What causes a leaky gut?
Intestinal permeability can be influenced by many factors, including
- gut inflammation (from infection, SIBO or dysbiosis)
- chronic stress and altered vagal tone
- diets low in fibre or high in ultra-processed foods
- alcohol and NSAID use (e.g. ibuprofen)
- microbial imbalance, especially reduced butyrate producers
- underlying conditions such as IBD or coeliac disease
These influences can compromise the tight junctions between cells, disrupt the gut environment and reduce the barrier’s ability to regulate what passes through.
Can you test for leaky gut?
There are a few ways to assess intestinal permeability, the most established being the lactulose-mannitol urine test, which measures how well different-sized sugar molecules pass through the gut lining. Stool zonulin is sometimes used as a marker, though its reliability and clinical utility remain debated.
In practice, these tests aren’t always necessary—or available—for every case. While they’re the only way to formally assess permeability, experienced practitioners can often form a working hypothesis based on
- symptoms
- risk factors
- inflammatory patterns
- microbiome imbalances
This approach isn’t diagnostic, but it can help guide a supportive protocol when a disrupted barrier is suspected.
How to support the gut barrier
You don’t need a diagnosis of “leaky gut” to support your gut lining—it’s something most people can benefit from. Rather than focusing on a single supplement, a broader, ecology-based approach is often more effective:
- Feed your microbes– fibre and prebiotics (like PHGG, GOS or inulin) help butyrate producers thrive, which is key for barrier integrity
- Reduce gut stressors– cut back on alcohol, ultra-processed foods and unnecessary medications where possible
- Address dysbiosis gently– restore balance rather than aggressively wiping microbes out
- Support the mucus layer– nutrients like zinc, glutamine and polyphenols (e.g. from berries or green tea) may help maintain barrier structure
- Manage stress– vagal tone and nervous system balance influence barrier function more than most people realise
The bottom line
The gut lining is a dynamic, intelligent barrier—designed to be selective when nourished, supported and functioning optimally. While increased permeability may contribute to a range of health concerns, it’s rarely the sole driver. Addressing it thoughtfully, in the context of the whole ecosystem, is what makes the real difference.
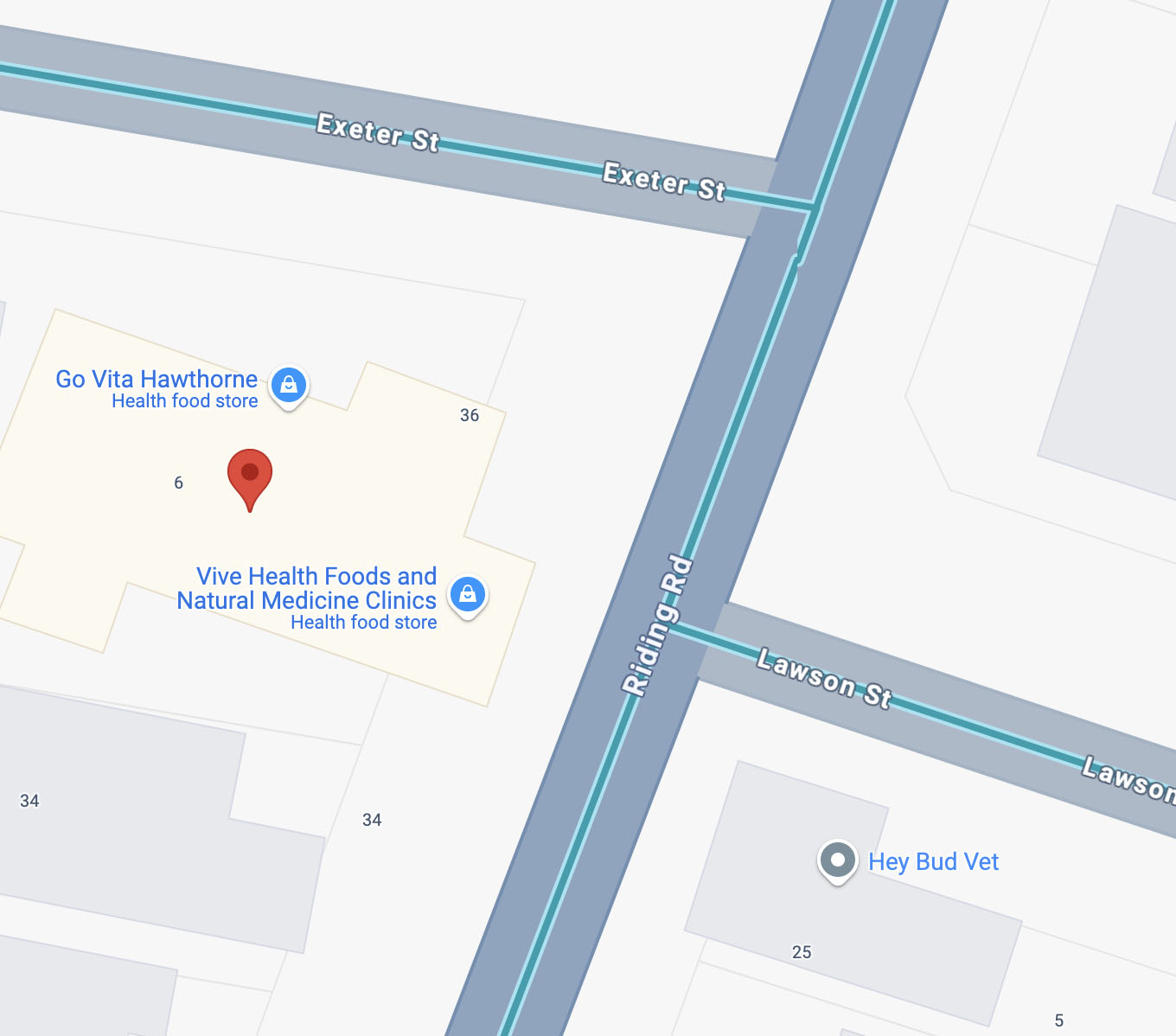
If you’re curious about how to support your gut barrier—or you’ve been wondering whether your symptoms could be linked to permeability—our in-store team at Vive Health can guide you with personalised, evidence-informed advice. For more complex cases, you can book a consultation with one of our practitioners at www.viveclinic.com.au
Article written by
Peter Christinson
BHSc (Nutritional and Dietetic Medicine)
Retail and Clinic Manager